Addison’s Disease
What is Addison’s disease?
Addison’s disease is a condition that affects your body’s adrenal glands. These glands are located on top of your kidneys. They make hormones that affect your mood, growth, metabolism, tissue function, and how your body responds to stress.
Addison’s disease damages those glands. It causes your body to shut down production of the hormones. The disease commonly affects people 30 to 50 years of age. However, it can occur at any age and affects both men and women.
Symptoms of Addison’s disease
Symptoms appear over a period of several months. They are difficult to diagnose because they are vague. Symptoms include:
fatigue
muscle weakness
joint or muscle pain
fever
weight loss
nausea, vomiting, and or diarrhea (leading to dehydration)
headache
sweating
changes in mood or personality, such as irritability, anxiety, or depression
loss of appetite
darkening of the skin (called hyperpigmentation)
lightheadedness or fainting when standing up, due to low blood pressure
cravings for salty food
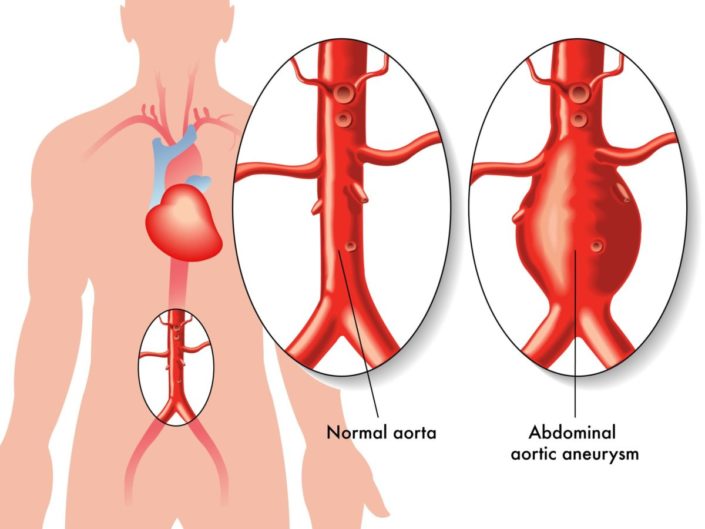
sudden, severe pain in the abdomen (lower stomach), lower back, or legs
confusion or slurred speech
sluggish movements
seizures
high fever.
When symptoms appear suddenly, or quickly get worse, it is called acute adrenal failure. Sometimes it’s called Addisonian crisis. This can lead to death if not treated. If you have any of the following symptoms, contact your doctor or go to an emergency room immediately.
sudden, intense pain in your lower back, abdomen, or legs
severe vomiting and diarrhea (which will lead to dehydration)
lower than normal blood pressure
unconsciousness
high levels of potassium and low levels of sodium.
What causes Addison’s disease?
Addison’s disease is caused by injury to your adrenal glands or when your glands are affected by another medical condition. This is called adrenal insufficiency. There are 2 types of adrenal insufficiency:
Primary adrenal insufficiency: This occurs through damage to your adrenal glands by an autoimmune disease (when your body attacks its own immune system). Other causes of primary adrenal insufficiency include:
Tuberculosis (or other infections) of the adrenal glands
Cancer of the adrenal glands
Bleeding of the adrenal glands
Secondary adrenal insufficiency: This occurs when another condition causes the adrenal glands to stop producing hormones. For example, a problem with your pituitary gland can cause secondary Addison’s disease. Or, you may develop Addison’s disease if you suddenly stop taking a corticosteroid medicine (such as prednisone). Corticosteroids are sometimes prescribed to treat conditions such as asthma, allergies, arthritis, cancer, and immune system problems.
How is Addison’s disease diagnosed?
Your doctor will ask you about your medical history and your symptoms. He or she may also perform laboratory tests to determine whether you have Addison’s disease. Those lab tests include:
Blood tests to measure your body’s hormone and mineral levels. Your doctor may check your blood before and after an injection to see if your body is responding normally to increased levels of certain hormones.
Computerized tomography (CT) scan or magnetic resonance imaging (MRI) to look at the size of your adrenal glands or pituitary gland. These scans are similar to an X-ray.
Can Addison’s disease be prevented or avoided?
Addison’s disease cannot be prevented or avoided.
Addison’s disease treatment
Treating Addison’s disease usually involves taking prescription hormones. This can include hydrocortisone, prednisone, or cortisone acetate. If your body is not making enough of the hormone aldosterone, your doctor may prescribe fludrocortisone. These medicines are taken every day by mouth (in pill form).
Your doctor may also recommend that you take a medicine called dehydroepiandrosterone. Some women who have Addison’s disease find that taking this medicine improves their mood and sex drive.
If you are experiencing an Addisonian crisis, you need immediate medical care. The treatment typically consists of intravenous (IV) injections of hydrocortisone, saline (salt water), and dextrose (sugar). These injections help restore blood pressure, blood sugar, and potassium levels to normal.
Living with Addison’s disease
Living with Addison’s disease involves learning to live with the unpleasant symptoms. In addition, you need to prepare for the possibility of Addisonian crisis. This is a medical emergency that requires you to:
Carry a medical alert card and bracelet at all times. This gives emergency medical workers information about your condition.
Keep extra medicine with you in case you forget to take your medicine. Ask your doctor for an injectable form of corticosteroids for use in an emergency.
Tell your doctor if your symptoms change or if your medicines stop working the way they used to.
Questions to ask your doctor
Is Addison’s disease hereditary?
Can the severity of my symptoms get worse over time?
Is Addison’s disease rare?
Can Addison’s disease cause long-term kidney failure?
Resources
National Institute of Diabetes and Digestive and Kidney Diseases, Adrenal Insufficiency & Addison’s Disease
U.S. National Library of Medicine, Addison’s Disease